A story from the field: the day safeguarding became real

During a discovery project, I was visiting education settings across England to run in‑person research. That meant working inside real-world constraints: safeguarding processes, visitor protocols, staff availability, young people moving through corridors, rooms that suddenly became unavailable, and the constant awareness that you’re a guest in someone else’s environment.
At one site, we were told (almost casually) that more than half the staff were off sick with COVID, and another bug was doing the rounds. The cherry on top was that we were crammed into a small basement room that was colder than the rest of the building, so no ventilation, and a very high chance of catching whatever was circulating.
Two days later, I was ill. I stayed ill for weeks. I couldn’t take sick leave due to tight deadlines and stakeholders picking on any leave taken as “delaying the project”.
That was my reminder that:
Safeguarding isn’t only about what happens in the session. It’s also about what happens around the session: infection risk, travel load, lone working, fatigue, access, and the logistics nobody puts on the Gantt chart, including allowance for sick leave.
And if you think that’s “just wellbeing” …well, it isn’t. It’s research quality. When researchers are depleted, rushed, anxious about getting to the next site, or taking avoidable health risks, the work gets worse. Decision-making gets shakier, debriefs get skipped, boundaries blur, and the conditions for ethical, high-quality research quietly erode.
The safeguarding plan template I share with you (at the end of this article) is informed by what I now call “interesting” field notes (though at the time, they were mildly psychosis‑inducing events!). I’m sharing 7 field notes to set the stage for why (and I cannot emphasise this enough) a safeguarding plan really matters.
Field note #1: the invisible entrance
On one visit, I arrived at what looked like a massive establishment, but couldn’t find the entrance. Construction work, temporary buildings, and exactly zero signposting added to the pain. I spent the first 15 minutes convincing myself I’d come to the wrong place, while my Uber driver (now a distant memory) had left me in what felt like a no-man’s-land.
I rechecked Google Maps like 50 times, reread my emails and tried contacting the reception by calling but no luck.
Eventually, a stranger appeared, also going to the same place, pointed me to the entrance like a human “you are here” sign. It was like going through a maze!
No one had done anything malicious in this case. I’d sent confirmation emails. They’d replied. We’d all behaved like professionals. But nobody had thought to say:
“Entrance is currently around the back, follow the temporary fencing and come through the metal gates where all the clinical waste bins are lined up, and ignore the sign that lies.”
It wasn’t their “fault”. It was the assumption that got me. I did not treat basic navigation and access as part of safeguarding. The fix, is boring and brilliant:
Ask for photos of the entrance, a named contact with a mobile number, and a plan for what happens if you can’t get in within 10 minutes.

Field note #2: the lone working
When I was a PhD researcher, my office was in what was called “the Pink Building.” A large, light‑pink shed on campus. It had the architectural charm of a storage unit and the safety profile of, let’s say, “optimistic”.
One evening, we were preparing for a large-scale randomised controlled trial. We were printing and packing hundreds of consent forms, participant information sheets, and supporting documentation (ethical approval, what you need to know etc.). The kind of admin tasks that convinces you that your PhD is mainly an advanced qualification in stapling and packing envelopes.
Due to the looming deadline, I stayed late. A few others stayed late too.
At some point, without noticing, I became the last person in the building. And for some reason the main door would not open. I was stuck, and it was way past lone‑working hours. There were no CCTV cameras inside the building, and the dread of my supervisor finding out (and then them getting in trouble) was doing a lovely little duet with my panic response.
I called a friend who lived nearby. Luckily, they were home and they came and got me out.
Weeks later, I found out a different office in that same building had caught fire because a student smoked inside a wooden shed and left a still‑lit cigarette butt in a bin full of paper. The fire alarm did its job (thankfully). However, the final-year PhD student’s work couldn’t be rescued.
I’m sharing this because it’s the most predictable safeguarding lesson in academia (and beyond):
Lone working isn’t a badge of honour. It’s a risk that needs a plan.
Field note #3: the re‑traumatisation
Now for the one that still makes my eye twitch.
There was an opening event for a trial involving eating disorders. An influencer with lived experience was invited (paid to attend by public funding!). A media presence was expected. The senior investigator bragged about having “useful connections” in high places (because nothing says “scientific rigour” like name‑dropping your minister cousin).
Thank goodness the broadcaster didn’t show up, and neither did the “very important cousin”.
But what did happen was worse in a quieter way: there were clearly people in the room being impacted by the choices made around food, messaging, and the theatre of it all. It was a masterclass in how a team can be so focused on “PR” that they lose sight of basic emotional safety.
Putting large quantities of food and drinks in front of people (including the influencer herself) was not thoughtful. It was triggering for many because they were there due to lived experience of battling severe eating disorders that included anorexia, bulimia and so on… and then you have staff enthusiastically eating and drinking through it all.
That experience sharpened a point I now say out loud in project kick-offs:
You can have all the ethics paperwork in the world. If your team culture treats re‑traumatisation as an abstract risk rather than a real human outcome, you don’t have safeguarding, you have compliance cosplay.
And if the most senior person is the risk, you need a pre-agreed speak‑up route (not just “be brave”). A stop rule. A named escalation contact outside the immediate hierarchy, and a culture where safeguards are rehearsed, not improvised. In academia, the ethics board that approved the study is one route of escalation.

Field note #4: the day the institution-to-institution relationship collapsed
Here’s a scenario I wish more safeguarding plans covered: governance collapse.
I once travelled across the country for fieldwork in a healthcare setting. Everything looked “approved” on paper. Then I arrived, and suddenly I had no access. Nobody would speak to me and I was told to wait in reception for hours. Doors that should have opened didn’t. The relationship between the university and the partner organisation had fractured at a senior level, and I’d been left out of the loop.
So there I was with wasted travel cost, time, energy, preparation and a hard stop. This is safeguarding too.
Because safeguarding is also about protecting the work and the researcher. If a breakdown in institutional comms can strand you physically, professionally, and emotionally (and sometimes financially), then it needs to sit in the risk register like any other operational risk.
The question we rarely ask is who covers what? Before I now travel for fieldwork, I confirm insurance/indemnity and cancellation rules:
- who covers travel costs if access collapses,
- whether professional indemnity/public liability applies (especially if contracting), and
- who has authority to pause/stop fieldwork if safety conditions change.
Field note #5: families as a risk variable
In social care settings, there’s another layer that rarely makes it into tidy templates:
Families can be protective and brilliant, and they can also be chaotic, accusatory, and sometimes actively harmful.
During my time working in social care and in an NHS rehab service, I’ve seen families raise serious concerns that were absolutely legitimate and needed action.
I’ve also seen families create issues where there were none. And I’ve seen situations where family members were taking money from someone in care, then implying it was the setting’s fault or that the staff “didn’t do their job properly” and attempting to escalate formally.
As researchers, we don’t prosecute. But we do need to plan for:
- third‑party risk,
- allegations and counter‑allegations,
- reputational volatility,
- and the possibility that “what’s true” is not always clear in the moment.
Field note #6: when the VPN and firewall are so safe they break the research
In one organisation, we assumed the laptops provided would seamlessly connect to Wi‑Fi on sites being visited. Trust me when I say: they did not. The firewall and VPN were so secure that even the host IT team couldn’t troubleshoot the connection.
The result was that MS Teams wouldn’t run, recording didn’t work, and there was no built‑in audio recording on the laptop. I also didn’t have a dedicated work mobile, so using my personal phone to capture audio would have breached policy.
We defaulted to note-taking, but even that became an issue because uploads to the analysis tool kept failing. We ended up with an incomplete dataset and analysis that relied far too much on memory.
Safeguarding lesson here is that you need a pre‑agreed offline plan (confirming Wi‑Fi access arrangements and device/VPN constraints in advance of the visit, approved recording routes, secure note templates, and a contingency for when tech fails), especially in high-stakes/high-security settings.
Another important thing to note is that in high-security settings like prisons, secure mental health hospitals, and immigration environments, safeguarding escalates because power imbalance is built into the setting. Recording may be prohibited altogether, device access may be restricted or denied, staff may be present in the session impacting what is said and shared, and “voluntary participation” can be complicated. For such settings, your safeguards need to be even more robust and explicit like having a paired working and no lone-working at all.
Field note #7: not everyone is willing to participate
One of the biggest lessons I learned is that not everyone will participate, even when your intentions are good and your paperwork is flawless. In some communities, trust is not easy to earn.
I’ve turned up at settings where I simply couldn’t access the voices I came to hear. Some communities have rational reasons for being cautious: history, extraction, misrepresentation, and previous “research” that didn’t translate into change.
This taught me that refusal is data too, not a failure. Safeguarding here means:
Designing for cultural safety and voluntariness which may look like working through trusted community connectors, using culturally appropriate facilitators where needed, offering different modes of participation, and being explicit that saying “no” to participation has no consequences.

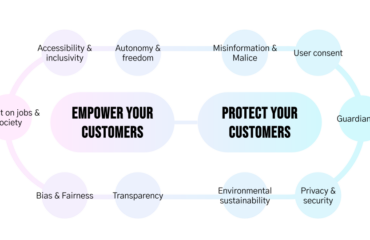
So… what is safeguarding, really?
Safeguarding is a delivery operating model, captured as a plan (or an agreement) that clarifies:
- who is responsible for what (and who makes decisions when conditions change),
- how consent and power dynamics are handled in real time,
- what we do if participant becomes distressed or discloses a risk,
- how we keep researchers safe (physical safety, lone working, travel, wellbeing),
- how we protect third parties (because research stories often include other people who haven’t consented),
- how we protect data, so insights don’t become unintended identifiers.
And crucially, how we execute the plan in real environments where everything is messy.
There are a few things that make a safeguarding plan comprehensive and fail‑safe
1) A trauma‑informed lens
Trauma‑informed approaches aren’t “extra sensitivity”. They’re pragmatic. They improve safety, choice, and trust, which tends to improve the quality of what people are able (and willing) to share.
In research terms, a trauma‑informed lens pushes you to design sessions where participants:
- know what’s coming,
- have meaningful control,
- can opt out without penalty,
- and aren’t pushed into disclosure “for the sake of insight”.
It also forces a professional acknowledgement that researchers can be impacted too by vicarious trauma, fatigue, stress, and the physical reality of operating in high‑pressure systems.
2) Factoring in incentives (as a safeguarding decision, not just admin)
Incentives can reduce barriers to participation, but they can also create pressure, bias, or risk.
I treat incentives as part of safeguarding:
- It must never be framed as “payment for disclosure”.
- It should not be conditional on answering every question or completing the session fully (especially in the digital world where 45 minutes into a 60 minute session, the connection breaks, or a participant faces issues when re-joining the session).
- It must be safe and discreet to deliver (cash can create risk; digital delivery can create privacy issues where emails, bank account details are shared).
- It should be equitable: if we pay for time, we should consider expenses and participation costs (travel, childcare, food etc.).
And yes, incentives can attract misrepresentation. People may tell you what they think gets them “into the study”, or what they think will please you. That’s not a reason to remove incentives; it’s a reason to:
- design screening carefully and thoughtfully,
- avoid recruitment through coercive gatekeepers,
- and be clear that incentives are not linked to “performing” as a good participant.
3) Consent and assent (done properly, not performatively)
This is the part that matters most, especially when vulnerable people are involved.
Consent for adults with capacity must be informed, freely given, specific, and ongoing (reconfirm at key moments).
Children: consent + assent
- Parental/guardian consent may be required (depending on policy and age).
- Child assent should still be sought even when an adult has consented on their behalf.
Assent is not a tick-box. It’s the child’s affirmative agreement, expressed in age-appropriate ways. And here’s what it may look like:
- If the child does not want to take part, verbally or non‑verbally, we stop.
- If the child wants to stop partway through, we stop.
- If the child wants to skip a question, we skip it.
No negotiation. No persuasion. No “just one more question.”
Vulnerable adults/adults who may lack capacity: supported decision‑making + assent
- Use supported decision-making (plain language, time, breaks, visuals, accessible formats).
- Check understanding by asking them to explain back (in their own words) what will happen, what will be recorded, and that they can stop.
If a person cannot understand/retain/weigh the information or communicate a decision even with support:
- you cannot rely on their consent alone,
- you may need a legally authorised representative process (depending on jurisdiction/policy),
- and you should still seek the person’s assent and monitor for distress or dissent.
And again: if they show they don’t want to continue, we stop.
Gatekeepers (who protect voluntariness)
Teachers, carers, clinicians, managers, and yes, prison staff, can enable access and unintentionally pressure participation. Build in:
- a private opt‑out route,
- clear “no consequence” language,
- and a cooling-off window where appropriate.
5 things I now do before I enter any setting (and why)
These are the “unsexy” steps that make fieldwork safer, and prevent heroics from becoming the plan:
1) Map safeguarding on both sides (and confirm clearance)
- Identify the host setting’s safeguarding lead and read their safeguarding policy before you arrive.
- Identify your organisation’s safeguarding lead and escalation route.
- Make sure both ends know how to reach each other quickly.
- Confirm clearance requirements early (e.g., enhanced DBS, prison/security vetting, NHS site rules). If clearance won’t land in time: pivot method early.
2) Build a fieldwork tracker (treat it like an asset, not admin)
Document:
- where you’re going (exact building location),
- photos of the entrance if it’s a complex site,
- who you’re meeting (names where appropriate, roles, agreed contact details),
- a named contact with a mobile number,
- timings, check‑in/out times, contingency routes,
- language requirements (do participants communicate in English; do you need an interpreter).
- Inform the setting that you’ll need to access their network and ask for WiFi and device connectivity early on so you avoid delays on the day.
- Create a separate tracker for your participants where you use participant IDs but keep participant contact details separate.
- Have a tracker for research work where you keep a record of what was recorded, with whom, who conducted the session, who took notes, who observed, what supplementary material was provided, if you upload the material and notes etc. For online research, you can adapt this tracker (links, time zones, backup numbers, “what if the platform fails”).
- For data security, upload to secure storage promptly, and don’t rely on “I’ll sort it later” when you’re travelling.
3) Treat public health as part of safeguarding (post‑COVID reality)
Before in‑person work:
- ask the site about outbreaks or visitor restrictions,
- confirm PPE expectations (even if “optional”),
- decide in advance what triggers a reschedule or a switch to remote.
4) Plan reset capacity like it’s a delivery constraint (because it is)
- Cap the number of intensive visits per week.
- Build half-day resets into schedules where needed.
- Protect debrief time as non‑negotiable (not a “nice to have”).
People who haven’t done fieldwork often only see the interview hour. They don’t see the off-stage work: ethics, documentation, travel (and all the drama of delays and connectivity), relationship management, safeguarding alignment, the emotional labour of holding space, and the operational coordination required to get usable data without harming anyone.
So if your team asks for frequent check-ins or expects you to do additional work, ensure that you set their expectations by walking them through all the off stage work needed.
5) Run a dynamic risk assessment on the day (including semi‑public spaces)
Conditions change fast: staffing, space, local incidents, illness levels, travel disruption. Your plan needs a mechanism for responding without stress.
And if you’re observing in semi‑public spaces (corridors, waiting rooms, receptions): plan for bystanders who didn’t consent. Decide what you record, how you protect privacy, and when you pause or reposition.
My template (use it and adapt it)
I’m sharing the template I now use as a default for discovery projects, user research and service design work across education, health, social care, pharmaceutical, justice, and other high‑stakes environments.
It’s intentionally written as a template: you’ll need to tailor it to your organisation’s safeguarding policy, ethics process, and the host setting’s local requirements.
If you’re working with children or vulnerable adults, you should always align the plan with the host organisation’s safeguarding lead and your own organisational safeguarding lead before fieldwork starts.
Safeguarding plan template for research (and design)
1. Document control
Table 1 shows the data fields that you can use for document control.

2. Purpose and scope
This plan sets out how we prevent harm, recognise distress or risk, respond to concerns (including disclosures), and learn from incidents. It covers:
- Participant safeguarding (physical, psychological, cultural, and digital safety)
- Researcher safeguarding (physical safety, psychological wellbeing, and lone-working)
- Safeguarding of third parties (people mentioned during research, bystanders, or dependents)
- Data governance and reporting practices that reduce risk and re-identification
- Decision-making for consent, capacity, and involving guardians or gatekeepers
- How participants raise concerns/complaints after participation (include contact details on information sheets and at session close)
3. Principles (proposed by
We adopt a trauma-informed approach and embed these principles into recruitment, consent, session design, data handling, analysis, and reporting:
- Safety (physical and psychological)
- Accessibility (physical and remote)
- Trustworthiness
- Collaboration
- Choice and transparency
- Empowerment
- Cultural considerations (including gender responsiveness)
- Recognising where there may be a potential for re‑traumatisation, and preventing it
4. Governance, roles and escalation
Define clear accountability and an escalation path so researchers can act quickly and consistently.
Roles (tailor):
- Safeguarding Lead/Designated Safeguarding Lead (DSL): receives concerns, decides next steps, liaises with statutory services
- Research Lead: ensures this plan is implemented, approves risk mitigations, oversees training
- Fieldwork Lead/Moderator (researcher on the ground): runs sessions, monitors distress, logs incidents
- Data Lead/Data Protection Officer (DPO): ensures secure handling, minimisation, and access control
- Partner/Gatekeeper Liaison: coordinates with schools/care settings/community organisations without coercion
Table 2 provides a worked example of an escalation map you can adapt and complete.

5. Risk assessment (before fieldwork)
Complete a safeguarding risk assessment for the topic, participant group, methods, and setting (in-person/remote). Use the risk matrix in Appendix A.
At minimum, assess:
- Sensitivity of topic and likelihood of triggering content
- Participant vulnerability (age, disability, trauma exposure, dependency, power imbalance)
- Setting risks (home visits, public spaces, care settings, online sessions)
- Researcher exposure (secondary trauma, lone-working, travel, hostility)
- Observers/note takers: their needs, triggers, and responsibilities (they’re part of the safeguarding environment too)
- Data risks (identifiers, recordings, storage access, retention)
- Third‑party risks (information about children/dependents/others)
- Language and culture as barriers to participation; plan accordingly
Additional in-person fieldwork risks (especially post‑COVID):
- Public health/infection-control risks (outbreaks, PPE/visitor rules, ventilation, hand hygiene)
- Clinical/biohazard risks where applicable (follow site infection-control protocols/training)
- Travel and fatigue risks (long days, commute safety, late finishes)
- Environmental/neighbourhood risks (area safety, transport availability, accessibility, lone travel after dark)
High-security settings (prisons/secure hospitals):
- restricted devices/recording, staff presence of in the sessions, coercion risk, emergency procedures, lockdown/incident response.
Plan for a dynamic risk assessment on the day.
6. Recruitment, screening, and participation support (including incentives)
Recruitment must be voluntary, proportionate, and designed to avoid coercion.
- Use plain-language invitations and information sheets
- Avoid recruiting via a person with direct power over the participant where possible (manager, teacher, clinician, prison staff). If unavoidable, add safeguards to protect voluntariness.
- Screen for immediate risk: if a participant is in acute crisis, signpost support and do not proceed.
- Plan accessible formats (easy-read, large print, multiple languages, captions)
Incentives, reimbursement, and participation costs:
- Equity: consider reimbursement for expenses and costs of participation (including for staff, service users, or people in custody, subject to policy).
- Document: amount, rationale, delivery route, timing, and what personal data is required to pay it.
- Confirm host policies: e.g., whether staff can accept gifts, and prison rules on incentives.
- Document potential issues: undue influence, misrepresentation, and how you’ll mitigate (neutral framing, ethical screening, opt‑out preserved).
7. Consent and capacity (adults, vulnerable adults, children)
Consent is ongoing, informed, and freely given. Use staged consent for recordings, artefact review, and attribution. Reconfirm at key moments.
Operational note: don’t assume digital consent will work. Bring printed packs for in-person sessions, or allow time at the start of remote sessions to complete consent. Confirm verbally and record confirmation; have a second team member witness if required.
Table 3 shows a worked example of a decision pathway that you can adapt.

Capacity checks (use appropriate local framework):
- Explain in a way the person can understand (visuals/easy read as needed)
- Check understanding (ask them to describe what will happen and their right to stop)
- If they cannot understand/retain/weigh/communicate a decision even with support, do not take consent from them alone
Provide complaints/concerns contact details on the info sheet and repeat at close.
8. Participant safeguarding during sessions
Build “safety by design” into every touchpoint.
Baseline safeguards:
- Content warnings and a plain-language roadmap
- “Menu of participation” (topics, depth, mode, anonymity)
- Choice throughout (breaks, camera off, written chat, skip questions)
- Use redacted/synthetic artefacts by default
- Normalise opting out without explanation
- Support signposting at start and end
- Avoid leading and probing language; also avoid pathologising terms
- Close with a grounding option if useful
Remote-session enhancements:
- Confirm participant is in a safe/private space; offer “switch topic” / “stop now” phrase
- Collect emergency contacts only where needed
- Use secure platforms; lock meetings; manage screen-sharing/chat safely
- If using an AI tool to record for later notes and analysis, inform the participant. Build that into your consent forms
- If remote observation is allowed, inform the participant. It’s unethical to allow a session to be watched by 10 observers via tools such as Marvin etc, while you introduced only one observer visible to the participant on MS Teams meeting. Build this into your consent materials and consent process
9. Managing distress, disclosures and safeguarding concerns
Distress script:
“Let’s pause here. We can take a break or switch topic. You’re in control, and it’s okay to skip anything. Here are support options if you’d like them.”
Disclosure script:
“I’m concerned this may relate to someone’s safety. I need to pass this to the safeguarding lead/DSL. I’ll note only what’s necessary and can help you contact them now.”
Incident recording: minimum necessary facts, no interpretation, store securely.
10. Researcher wellbeing and safety
- Pre-brief on trauma cues and de-escalation; rehearse scripts
- Buddy system for higher-risk sessions/field visits
- Time-box sessions; cap daily exposure; rotate facilitators
- Structured debriefs; document lessons learned
- Access to supervision/Employee Assistance Programme (EAP); encourage micro-breaks and recovery routines
- Lone-working check-in/out protocol and incident reporting
11. Data governance and reporting
- Collect minimum necessary detail; avoid identifiable case narratives
- Anonymise promptly; separate identifiers from research data
- Use quotes and video sparingly; approve sensitive quotes where appropriate
- Avoid sensational detail; focus on patterns and system insights
- Secure storage; limit access on a need-to-know basis
- Complete a Data Protection Impact Assessment (DPIA)/privacy assessment where required and ensure privacy notice is provided.
- Include a data breach escalation route (lost/stolen device, accidental sharing, unauthorised access).
12. Operating rhythm: before, during, after fieldwork
Before:
- Map triggers and design mitigations
- Prepare scripts for distress and disclosure; rehearse as a team
- Prepare referrals pathways/support signposting
- Prepare accessible materials; test with lived-experience reviewer where feasible
During:
- Begin with a grounding check-in; set norms (breaks, skip-anything, stop anytime).
- Monitor signs of distress; pause to check consent and comfort.
- If a disclosure relates to harm/risk, follow the incident pathway.
- Avoid rapid-fire questioning; allow silence and pacing.
After:
- Offer debrief and optional follow-up
- Provide support resources again
- Log incidents securely; confirm handover
- Build in team decompression and lessons learned. Have a research retro.
13. Monitoring, review and continuous improvement
Track adverse events and near-misses; review and update mitigations as the project evolves. Document learning for future studies.
Appendix A: Trauma‑informed risk matrix
Risk entry
- Risk/trigger:
- Who is affected: (participant/researcher/third party/organisation)
- Where it applies: (in-person/remote hybrid/specific setting)
- Likelihood: Low/Medium/High
- Impact: Low/Medium/High
- Early warning signs:
- Mitigation (before):
- Mitigation (during):
- Mitigation (after):
- Owner:
- Escalation route:
- Residual risk:
- Review date:
Appendix B: Session start scripts
B1) 1:1 session start script (copy/paste)
“Thanks for joining. Before we start:
- You can skip any question, take a break, or stop at any time.
- What you share will be treated confidentially, unless we become concerned about someone’s safety, in which case we may need to escalate via our safeguarding process. We will tell you if that happens.
- With your permission, we’d like to [record/take notes only]. You can change your mind at any time.
- If you’re receiving a thank-you for your time and participation incentive, it’s not linked to what you share or whether you complete the session.
If you have any concerns afterwards, you can contact:
- [Research Lead name + email + phone]
- Independent route (if available): [Ethics contact/host organisation contact]
Any questions before we begin?”
B2) Group session start script (copy/paste)
“Thanks for joining. Before we start:
- You can step out, skip any question, or stop at any time.
- We’ll ask everyone to respect privacy, but we can’t guarantee confidentiality in a group, please share only what you’re comfortable sharing.
- We’ll agree group norms to keep this respectful and safe.
- With your permission, we’d like to [record/take notes only]. You can change your mind at any time.
If you have concerns afterwards, you can contact:
- [Research Lead name + email + phone]
- Independent route (if available): [Ethics contact/host organisation contact]”
Appendix C: Incident and near‑miss log fields
(Facts-first. Minimum necessary detail.)
- Date/time:
- Mode: in-person/remote /hybrid
- Setting label: (non-identifying name)
- Reported by: (role)
- What happened: (facts only)
- Immediate actions taken:
- Safeguarding decision made:
- Escalation route used: (who was informed + when)
- People involved: (roles only where possible)
- Follow-up actions + owner:
- Closure date + notes:
- Learning captured/change to plan:
Appendix D: Fieldwork checklists
D1) Pre‑visit checklist
Safeguarding and governance
☐ Host safeguarding lead/DSL identified; host safeguarding policy reviewed
☐ Your organisation’s safeguarding lead confirmed + escalation route shared
☐ Speak‑up route confirmed (including stop rule if safety is undermined)
☐ Participant complaints/concerns route prepared (printed + digital)
Clearance/access
☐ DBS/enhanced disclosure/vetting confirmed where required (schools, NHS, social care, prisons)
☐ Insurance/indemnity confirmed for fieldwork (travel cancellation, liability, authority to pause/stop)
☐ Site security rules confirmed (badges, escorts, prohibited items, lockdown procedures if relevant)
Public health and safety
☐ Ask about outbreaks/visitor restrictions/PPE expectations
☐ Decide go/no‑go threshold (when you’ll reschedule or pivot)
Method + consent
☐ Consent and information pack materials prepared and sent (plain language, accessible formats, translations)
☐ Plan for consent capture issues: include printed packs for in-person; time in-session for remote
☐ Recording/photography rules confirmed (especially in education/prisons/clinical settings)
Incentives/participation support
☐ Incentive + reimbursement approach approved
☐ Host rules checked (staff gift restrictions; prison rules; voucher/cash constraints)
☐ Delivery method + minimum data required confirmed
Tech + data security
☐ Test Wi‑Fi/VPN implications if on-site devices are restricted
☐ Offline contingency ready (secure note template, approved recording route, backup plan)
☐ Device security: encryption, screen lock, storage route, deletion policy
Logistics
☐ Entrance details confirmed (photo/map); named contact with mobile number
☐ Travel plan + contingency (late arrival rules, cancellation trigger)
☐ Lone-working/buddy arrangements and check-in/out times set
☐ Interpreter booked if needed (and briefed on confidentiality + safeguarding)
D2) On the day checklist
☐ Sign in; wear ID; confirm where safeguarding lead/DSL is; fire/first‑aid rules
☐ Dynamic risk assessment completed (staffing changes, room changes, illness, incidents)
☐ Reconfirm consent + recording rules
☐ Restate ground rules: skip/stop anytime; confidentiality limits; complaints route
☐ Monitor distress; pause and re-check consent
☐ If concern arises: Stop → Listen → Record → Report (per escalation map)
High-security environments (add if applicable)
☐ Confirm escort requirements and privacy limitations
☐ Confirm what you can/can’t bring in (devices/chargers/notebooks)
☐ Confirm whether staff presence may affect voluntariness; add opt-out route
D3) Post‑visit checklist
☐ Securely upload notes/media to approved storage; remove local copies as required
☐ Log incidents/near‑misses; inform safeguarding lead/DSL as appropriate
☐ Team debrief (participant wellbeing + researcher wellbeing + lessons learned)
☐ Update risk register and safeguards based on what changed on the day
☐ Deliver incentive/reimbursements within agreed timeframe
☐ Send participant follow-up (thanks + signposting + complaints route reminder if appropriate)
Appendix E: Fieldwork tracker fields
(One entry per visit/session.)
- Date:
- Setting label:
- Full address (internal only):
- Entrance instructions + photo link:
- On‑site contact (name/role) + mobile:
- Host safeguarding lead/DSL (name/role) + mobile:
- Who you’re meeting (roles only):
- Method (interview/group/observation):
- Participant vulnerability flags (high-level only):
- Interpreter required? (Y/N)
- Recording allowed? (Y/N)
- Device restrictions? (Y/N + details)
- PPE/outbreak status confirmed? (Y/N + notes)
- Travel plan + contingency:
- Check-in time/check-out time:
- Buddy/escalation contact:
- Notes/risk flags:
Appendix F: Safety planning grid
(Pre-plan your “if this happens → we do this” responses.)
- If this happens: participant distressed
We will: pause; offer break/skip/stop; signpost; document near‑miss if needed - If this happens: disclosure indicates risk of harm
We will: explain confidentiality limits; record minimum facts; escalate to DSL - If this happens: researcher feels unsafe
We will: end session; exit safely; buddy check-in; incident log - If this happens: outbreak/illness risk escalates
We will: follow site rules; apply PPE; reschedule/pivot to remote - If this happens: tech prevents secure recording
We will: use approved backup plan (secure notes/approved device/reschedule)
Further resources:
- Trauma-informed social research: a practical guide. Fulfilling Lives South East Partnership. Great for running trauma-informed interviews, focus groups, and observations.
- HMPPS, Conducting research in prisons/probation/HMPPS (National Research Committee guidance). Practical entry point to prison research governance and application routes
- DfE, User Research Manual, Research with children and young people. Practical, research-specific guidance on planning and running research safely with under-18s, including incentives, consent, and safeguarding.
- A practical guide to trauma-sensitive research: integrating trauma-informed frameworks into the qualitative research lifecycle (2024)
Very on-point on how to design, run, analyse, and report qualitative research in ways that reduce re-traumatisation, including supervision and researcher wellbeing. - WHO Research Ethics Online, Guideline 15: Research involving vulnerable persons. Clear, global framing of protections without exclusion.
- Also look at safeguarding plans/policies created by various universities like the ones by University of London, Imperial College London etc.
Post‑COVID user research needs a revised safeguarding plan was originally published in UX Collective on Medium, where people are continuing the conversation by highlighting and responding to this story.